About Mycobacterial Diseases
Tuberculosis
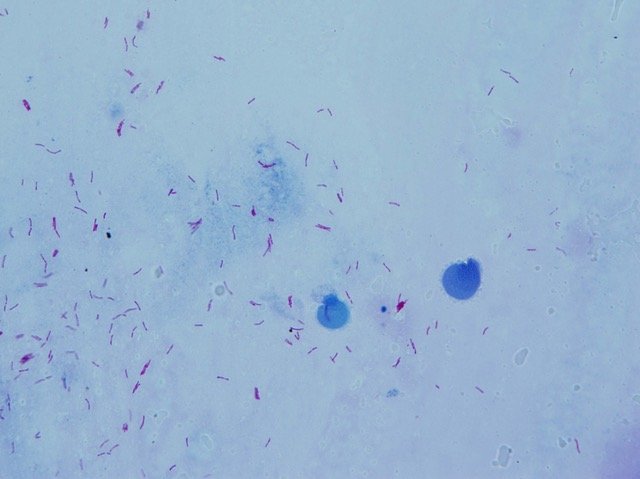
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis, primarily affecting the lungs, but also capable of causing lesions in other organs. Tuberculosis is spread from person to person through airborne transmission.
In many cases, the body's immune system successfully contains the pathogen, leading to a latent state and preventing symptomatic manifestation. However, if the immune system is weakened, the pathogen can become active, causing the disease. Symptoms of active tuberculosis include cough, sputum, hemoptysis, chest pain, fatigue, weight loss, fever, and night sweats. It is crucial to identify and treat individuals with tuberculosis, even if asymptomatic, to prevent further spread of the infection.
The diagnosis of active tuberculosis relies on pathogen identification, and a chest X-ray is also valuable for detecting pulmonary tuberculosis. Treatment for tuberculosis requires the use of multiple anti-tuberculosis drugs for a specified period of time. It is important to take the drugs regularly and as prescribed to complete the treatment and prevent relapse.
Recently, new drugs have been developed that can shorten the treatment period and reduce the need for injectable medications. However, tuberculosis remains a major problem in high-burden countries, especially in Asia and Africa. The co-infection of HIV poses a significant threat in some areas, and the spread of drug-resistant tuberculosis originally emerging from treatment interruption or incomplete treatment is a major global concern.
The BCG vaccine is given to infants in these countries, but its effectiveness in adults is limited. In recent years, the COVID-19 pandemic has caused significant delays in tuberculosis control. For the eradication of tuberculosis, there is a need for research and the development of novel tools effective in each phase of diagnosis, treatment, and prevention.
(Written by Naoto Keicho)
Leprosy
Leprosy is a chronic infectious disease with granulomatous lesions caused by Mycobacterium leprae and M. lepromatosis.
Due to its long doubling time (approximately 12 days) and low optimal growth temperature (30-32℃), leprosy causes granulomatous lesions mainly in the skin, peripheral nerves, eyes, and nasal and oral mucosa.
Dapsone, which was introduced as the first effective drug in the 1940s, followed by rifampicin and clofazimine in the 1960s, and multidrug therapy (MDT) in the 1980s, made leprosy a truly curable disease. New cases in Japan have been drastically reduced to almost exclusively foreign-born incidences.
However, the number of new cases worldwide has remained steady over the past decade or so at around 200,000 annual infections, focused mainly in India, Brazil, and Indonesia. Leprosy is still an infectious disease with challenges to be addressed, which include: the as-yet unsuccessful in vitro culture of M. leprae and the difficulty of preventing harm caused by leprosy reactions (severe allergic responses that mostly occur during treatment).
(Written by Manabu Ato)
NTM
and the urgent health concern
in Asia
NTM (nontuberculous mycobacteria) causes refractory chronic pulmonary infections, primarily affecting middle-aged and older women, as well as individuals with pre-existing lung conditions.
NTM, which are bacterial species prevalent in the environment (such as those in soil and tap water), have seen a recent increase in reported species. Notably, M. avium and M. intracellulare collectively form the M. avium complex (MAC), constituting approximately 90% of causative agents for pulmonary NTM disease in Japan. Noteworthy are emerging clinically problematic species like M. abscessus and M. kansasii.
Symptoms of NTM lung diseases (NTM-LD) comprise cough, sputum, and, in advanced cases, shortness of breath. However, the disease is often identified through abnormal chest findings during physical examinations, even in the absence of symptoms.
Symptomatic CT chest images are characterized by nodular bronchiectatic lesions in the middle lobe and the lingula (NB type). Conversely, the FC type, more prevalent in men with a smoking history, contrasts with the NB type, which occurs predominantly in thin, middle-aged women lacking pre-existing lung diseases.
The primary treatment involves a three-drug regimen comprising clarithromycin (or azithromycin), ethambutol, and rifampicin. Amikacin is administered intravenously three times a week, every other day, for a maximum of six months.
The incidence of NTM-PD in Japan has shown an escalating trend (Figure 1). Specifically, the rate was 5.6 cases per 100,000 people in 2007, jumping to 14.7 cases per 100,000 people in 2014. Within seven years, it more than doubled, surpassing the incidence rate of tuberculosis. This underscores the growing significance of NTM-PD as a contemporary health concern.
Figure 1. Incidence rate in Japan (Namkoong, Ho et al. (2016). Epidemiology of Pulmonary Nontuberculous Mycobacterial Disease, Japan. 22(6).)
On the other hand, in most countries, the incidence rate of NTM-PD is not estimated (Figure 2). Currently, there are cases where individuals with NTM disease are misdiagnosed as having tuberculosis due to the similarities between the two illnesses. Additionally, the lack of access to laboratories may result in the inability to conduct necessary tests, leading to situations where NTM diagnosis and treatment are not being carried out. Therefore, understanding the true prevalence of NTM, including the actual number of NTM-PD patients, has become an urgent challenge.
(Written by Ho Namkoong)
Figure 2. Countries where NTM disease surveys were conducted (Dahl, V. N., Mølhave, M., Fløe, A., van Ingen, J., Schön, T., Lillebaek, T., ... & Wejse, C. (2022). Global trends of pulmonary infections with nontuberculous mycobacteria: a systematic review. International Journal of Infectious Diseases, 125, 120-131.)

